Parathyroid Disorders: Causes, Symptoms, and Treatment Options
Understanding Parathyroid Disorders
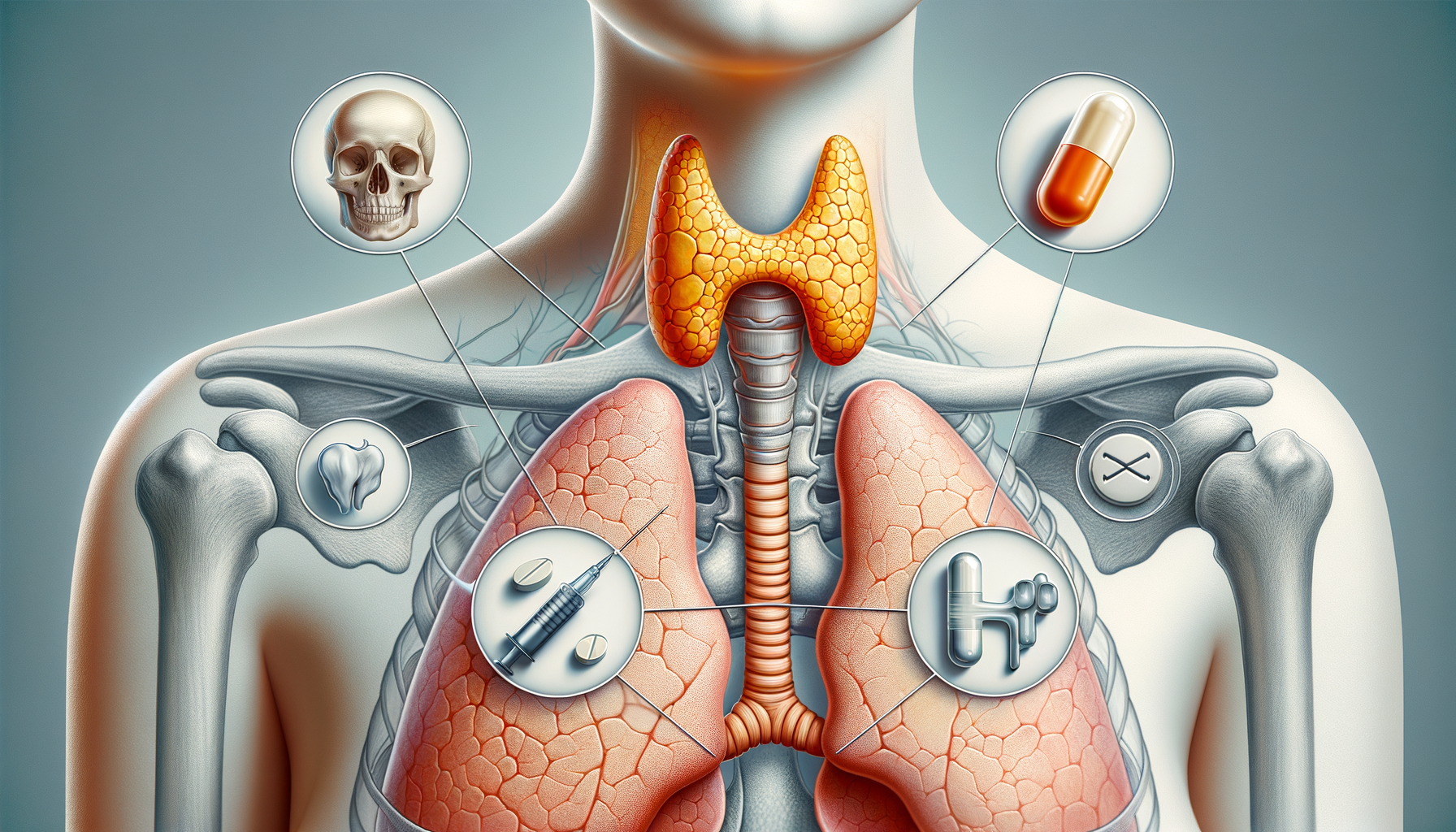
The parathyroid glands, though small, play a crucial role in maintaining calcium balance in the body. These four tiny glands located behind the thyroid produce parathyroid hormone (PTH), which regulates calcium levels in the blood. Parathyroid disorders occur when these glands produce too much or too little PTH, leading to hyperparathyroidism or hypoparathyroidism, respectively. These conditions disrupt the delicate balance of calcium, which is vital for bone health, muscle function, and nerve signaling.
Hyperparathyroidism is characterized by excessive production of PTH, often leading to elevated calcium levels in the blood, a condition known as hypercalcemia. This can result in symptoms such as fatigue, bone pain, kidney stones, and increased thirst. Conversely, hypoparathyroidism involves insufficient production of PTH, causing low calcium levels, or hypocalcemia, leading to symptoms like muscle cramps, tingling in the fingers, and even seizures.
Understanding the underlying causes of these disorders is essential for effective treatment. Hyperparathyroidism is often caused by benign tumors on the glands, known as adenomas, or enlargement of the glands. Hypoparathyroidism may result from surgical removal of the glands, autoimmune diseases, or genetic factors. Early diagnosis and treatment are crucial to prevent complications and improve quality of life.
Diagnosis and Evaluation of Parathyroid Disorders
Accurate diagnosis of parathyroid disorders involves a combination of clinical evaluation, laboratory tests, and imaging studies. Clinicians typically begin with a thorough medical history and physical examination to identify symptoms indicative of calcium imbalance. Blood tests are crucial for measuring calcium, phosphorus, and PTH levels, providing insight into the gland’s functionality.
For hyperparathyroidism, elevated calcium and PTH levels are indicative of the disorder. In contrast, hypoparathyroidism is diagnosed through low calcium and PTH levels. Imaging studies, such as ultrasound or a Sestamibi scan, may be employed to locate abnormal parathyroid glands or tumors. These diagnostic tools are essential for determining the appropriate treatment approach.
In some cases, genetic testing may be conducted to identify hereditary forms of parathyroid disorders. This is particularly important for individuals with a family history of the condition. The comprehensive evaluation not only aids in diagnosis but also helps in tailoring individualized treatment plans to address specific needs and prevent potential complications.
Treatment Options for Hyperparathyroidism
Treatment for hyperparathyroidism primarily focuses on reducing elevated calcium levels and addressing the underlying cause of excessive PTH production. Surgical removal of the overactive gland or glands is often the most effective treatment. Known as a parathyroidectomy, this procedure is highly successful in normalizing calcium levels and alleviating symptoms.
For patients who are not surgical candidates, medication may be prescribed to manage calcium levels. Calcimimetics, for instance, can mimic calcium in the blood, thereby reducing PTH secretion. Additionally, bisphosphonates may be used to protect bone density, a common concern in hyperparathyroidism.
Lifestyle modifications, such as staying hydrated and maintaining a balanced intake of calcium and vitamin D, are also recommended to support overall health. Regular monitoring of calcium levels is essential to ensure the effectiveness of treatment and to make necessary adjustments.
Approaches to Managing Hypoparathyroidism
Treating hypoparathyroidism involves restoring calcium levels to normal and addressing symptoms. Calcium and vitamin D supplements are the cornerstone of treatment, helping to maintain adequate calcium levels and prevent complications such as tetany and seizures.
In some cases, recombinant human parathyroid hormone (rhPTH) may be prescribed to replace the deficient hormone, offering a more physiological approach to treatment. This therapy is particularly beneficial for patients who do not respond adequately to conventional treatments.
Regular follow-up and monitoring are crucial to ensure optimal calcium levels and to adjust treatment as needed. Patients are often advised to wear medical alert bracelets and to be aware of symptoms indicating low calcium levels, such as tingling or muscle cramps, to seek prompt medical attention.
Living with Parathyroid Disorders: Patient Perspectives
Living with parathyroid disorders can be challenging, but with appropriate management, individuals can lead healthy lives. Education and awareness about the condition are vital for patients and their families. Understanding the symptoms and treatment options empowers patients to take an active role in their healthcare.
Support groups and patient communities offer a platform for sharing experiences and coping strategies, providing emotional support and encouragement. Engaging in regular physical activity, maintaining a balanced diet, and adhering to treatment plans are crucial for managing symptoms and preventing complications.
Regular communication with healthcare providers ensures that treatment plans remain effective and that any changes in symptoms are promptly addressed. With the right support and management strategies, individuals with parathyroid disorders can navigate their health journey with confidence and resilience.